The Spark: Why
I became interested in surrogacy almost ten years ago when a loved one struggled to have a baby. I considered offering to carry a child for her; however, just before I was to offer, we got the news. After years of failed attempts including IVF, she miraculously conceived…. twins! It was such a blessing for her family, which then put surrogacy out of my mind until two years ago when my close friend disclosed that she had done it and was in the process for her second go-round of the journey. Again, it weighed on my heart and curiosities to embark in this adventure. I prayed. I talked with my mother- my spiritual comrade- about the biblical implications of this decision. I earned her blessing, which was vitally important to me. Yet, I dragged my feet because foolishly I had hoped that my best guy friend who desperately wanted a baby girl would stop joking that we “make a baby” and seriously ask me. Then my life got busy… It wasn’t until December 2020, when my friend said she’d give my info to the agency, that I truly let God take the lead. Lord, let this gift of love flow freely.

2014: My Bathtub Baby
The Stipulation: What’s Important
After having three children of my own, I experienced the importance of nursing upon delivery. The hormones that are released help to close or tighten the organs and enable me to heal faster. The colostrum/first milk are extremely valuable to the baby’s development. Therefore, the stipulation in finding a couple was that they must allow the baby to be breastfed after delivery.
Nursing is a time of bonding for the mother and child; however, this is not my child. The mother-to-be may become fearful that I am bonding with her child and not want this to occur. However, I see the act as a very practical time meant for biological benefits for the surrogate and the child. Even with my own children, bonding took time- rich with new experiences and personality development. I hope that expressing the practicality of it will ease the trepidations of the new mom.
The Three That Mean the World:
“Mom, if I can’t have a baby when I’m older, will you have it for me?” Of my three, my middle girl (i.e., 8 years old) is the most interested in the process. She asks me almost everyday when I’m going to “get a fat belly” with a baby. We’ve watched videos of the meaning and process and she clearly understands that we will not be keeping it when it arrives… Her enthusiasm is contagious!
My friend, on the only hand, reserves the right to share the experience with her young children until after the first trimester and well into “the safety zone.” I completely understand and respect her decision; however, I wish I had known that fact prior to telling her 8-year old that I was going to be a surrogate too. I had to backtrack my statements when she said, “What? My mom’s pregnant and didn’t tell me!” Oops.

Prepping for Pregnancy
Only one of mine was planned. And nope, it wasn’t my first. I didn’t know to take prenatal vitamins in the months leading to conception because conception was the furthest from my mind! But now I’ve wised up. As soon as I made the decision, I marched myself down to the pharmacy to pick a packet of a prenatal prescription (just kidding, it was a non-Rx bottle from a large corporate retailer… come on… just let me have the alliteration!). The next step, stop with the birth control. So… I had my IUD removed in January… Now fellas, don’t come knockin’ down my door! I’m saving myself.

About Me
Hi, I’m Aaron. I have three children of my own. They are beautifully crafted gifts from God. I cannot imagine life without our connection, love, laughter, and struggles. This journey is not only for me, it is a family experience that will last a lifetime!
Subscribe to My Blog
Get new content delivered directly to your inbox.
The Couple
It all happens so fast. They told me to expect a same-sex couple due to my stipulation about breastfeeding. “Great!” I said. I’m here for the experience of giving one of the most- if not the most- precious gift to a couple who wish to love a child! Then I got the email about The Couple: Now for the sake of their privacy, I will not be divulging any information about them, but it would be nice to give them names… Ah yes…
"My father’s name was Walter Shirley, and he was a teacher in the Bolingbroke High School. My mother’s name was Bertha Shirley. Aren’t Walter and Bertha lovely names? I’m so glad my parents had nice names."
-Anne Shirley
From Lucy Maud Montgomery’s classic Anne of Green Gables
We shall refer to them as Walter and Bertha. Such lovely and distinguished names, don’t you think? They were humble and sweet and didn’t mind my American exuberance.
In this process there is no time wasted: We got right into the discussion of nursing. “Bertha” admitted her qualms- rightfully so, any mom would be hesitant- but was willing to work out a plan so that we are all comfortable. Shortly after our video conference, I got the text: They liked me! They want to move forward.
Details, Details, Details
This process doesn’t start with an egg nor a sperm. It starts with legal, escrow, insurance, and IVF clearance.
The funds are held prior to matching with a surrogate. Monies will be reimbursed for the typical expenses of being pregnant and any needed time off work. These are in addition to the “rental fee” of my cozy warm uterus.
For the last several months, I only had my student insurance because I am now an independent contractor with my work (thus no company benefits). I have been researching policies and wondering which one would be best for someone “trying to conceive” but not yet pregnant? Yet when I’m faced with so many choices, I freeze. So I was surprised and equally thrilled to get the email stating that their contact would be working with me to set up an insurance policy that they had already chosen for me! YES!!! Not only that, “I am sending you the funds to pay for it.”
I took off work to visit the IVF clinic in March. It was a lovely sunny day to smell the salty breeze near the ocean, so I also treated myself to brunch at an iconic eatery. At the clinic, they took vials of blood, a urine sample, and examined the walls of my uterus. Everything checked out A-Okay! About a week later, I received the official medical clearance, despite a slight insufficiency in my Vitamin D level. Next, I was to start taking low-dose aspirin, 2000 IU of Vitamin D, continue with the prenatal vitamin, and start the pill on the second day of my next period (so they could have greater control over the cycle). After each step, I think, “Wow, I’m really doing this! I’m one step closer to carrying someone’s child!”
In the beginning of April, I reviewed the first draft of the contract with my attorney. We added the nursing request and stipulated that a C-section would be a last resort. Also, although I am open to other necessary vaccinations, I declined the COVID vaccine. There’s just not enough information yet, especially for an unborn fetus; therefore, I will continue to follow the guidelines set by the CDC so that the baby and I remain safe. The legal contract also contained other details of the surrogacy plan and participants’ rights/responsibilities. My attorney made a few proposed changes and now their lawyer will review it with them. We’ll deliberate until both parties are comfortable with the plan. Our final terms will be ironclad- unless anyone’s got a diamond (blade that is).
Finally, I will begin the medications prior to implantation.

Scampering Boulders in Joshua Tree NP

Medications
I am usually not one who takes prescription medications because I prefer natural remedies and methods. I didn’t mind taking “the pill” for a few weeks but was glad when I was able to stop because it tends to give me these “reality shifts” that are like vertigo. I also have to take estrogen daily. After starting this one, I noticed having more anxiety-type bubbles in my chest. I just need to lay down and breathe when that happens. It passes quickly. The big one has been progesterone INJECTIONS. Yes, that’s why, I’ve started shooting up. I was incredibly nervous the first time I did it. I don’t have a problem with needles (I like to watch the nurse do it), but I haven’t used one on myself. I didn’t fear the pain. I feared that I would get an air bubble in there or stick it in wrong. I had two videos for reference, which were extremely helpful. My surrogate friend also offered to help. But I thought, I’m a strong-ass woman… I can do this! I prepped the injection site, added the progesterone oil to the syringe, switched needles… but when I was trying to get the cap off the second needle, it slipped and stuck me three times in the fingers. Honestly, I have no idea how it got me 3 times! hahaha. So, then I had to deal with blood everywhere while trying to keep going with my mission of sticking my butt. I twisted my torso around to find the best spot- 90 degree angle- and push. It went through like “buttuh.” The injection site was tender for several days- way more than the other sites the next days. I wondered if this was because I did it a bit too far back or was it because there may have been something from the finger prick inside the needle. Interestingly, the spot on my fingers was bruised for a few days after but the injection sites were not. But… all in all… I made it through.
Embryo Transfer
I was nervous about the embryo transfer. Would it feel weird to have a foreign life force implanted in my womb? However the nurses put me right at ease with all the information about the procedure and how the embryo had progressed during the thawing process. Finally, the lights dimmed, patient and embryo identifications were repeated, the tube that ran through a small door in the wall was the passageway for new life, a voice over the intercom confirmed that “the embryo is ready for transfer.” It was quick, painless, and brought joy to the intended parents who viewed the procedure over a video conference call.
Despite feeling like it would drop out when I walked, the doctor assured me that it wouldn’t. I rested for 10 minutes then was able to return home for bedrest while my body adjusted. The kids were a great help in getting anything I needed… and perhaps I took advantage of that…. just a little.
The 1st Trimester
Exhaustion. The first trimester made me feel like I had chronic fatigue. Thankfully it was summer and I didn’t have work. On the bright side, I never experienced morning sickness. It was a pleasant feeling when we saw and heard the heartbeat for the fist time. It brought such joy to the intended parents. It was such a relief to me that the pregnancy had been a success. My fear was that I would disappoint the intended parents with it not “taking” to my body.
My plan was to stay in town during the pregnancy; however, my mom broke her femur and I needed to drive 12 hours across state lines to be with her. This required written approval from my doctor. I had graduated from the fertility clinic but due to an insurance snafu, I had not gotten an appointment with my OB. However, the fertility clinic was able to see me once more to gain approval to leave the state (per my contract). The ultrasound showed a healthy baby of 9 weeks. My visit was a delight and I was able to eat fresh greens from the garden each day. My energy level was very low, but maybe that was because I had stopped drinking coffee as a wakeup remedy in the mornings… instead I drank hot almond milk.
When I got home around 10 days later, I had to resolve a situation with my pets. On Friday it was my 12 week mark and was my last day for the progesterone injections and estrogen pills. On Sunday, while waiting for the vet, I experienced some light-to-moderate cramping in my lower abdomen. I thought perhaps it was indigestion or needing to have a bowel movement. However, when the vet assistant came out to talk with me, I stood up and took a step, and felt as if I had a water break. I hoped that I had just peed my pants (not ever would I wish that except for in a situation such as this). I had a dress on and didn’t feel anything dripping down my legs so I had to grin-and-bear it while I finished the conversation, paid, and retrieved the kittens from their care. Thankfully, I had an old towel in the truck to put on the seat while I drove home. When I got home to the toilet, I realized it was a mess of watery blood. I immediately put myself on bedrest and texted the agency to see if this was a normal side effect of stopping the progesterone injections and estrogen pills. I asked them if they thought this was a reason to go the urgent care or ER. They assured me that it was normal to have some bleeding during early pregnancy and that bedrest would suffice. They also said that it could be the pocket of fluid that gets trapped during the embryo transfer and needs to be released eventually. After a few days, I felt better.
The 2nd Trimester
Yet, I didn’t feel relief. My mind was left with what ifs. I couldn’t just see my OB because of the insurance issue so I continued to jump every hurtle and chase every wild goose to resolve that issue… so I could see a doctor! Eventually, I changed the group, got the authorization, and waited for a call back from the OB’s office. Because they are just awful at returning calls, I decided to go in to make my appointment. However, the earliest they could see me was in roughly two to three weeks, which would put me at 16.5 weeks. I accepted the first available appointment and asked to be on the list if there were cancellations. It was frustrating to not be seen between 9 and almost 17 weeks but due the insurance difficulty, I had little choice.
I continued to worry. What if it wasn’t alive? Am I losing weight or just my mind? I just want an ultrasound to hear a heartbeat. I called several urgent care centers but no one had an ultrasound machine. I considered the ER but felt that it wasn’t really an emergency. I had to just wait for the appointment. Finally, I requested an appointment online at the hospital maternity unit. While I waited for their response, the surrogacy agency (knowing my concern and difficulty with getting an appointment) suggested a 4D ultrasound. I made the appointment on Wednesday to be seen on Friday.
The End of Life
I did everything I thought I could to be seen. Even though I really tried to think positively, my intuition kept bringing me back to…. something’s not right. I prayed in vain because something in me said, it’s gone. But I wanted to ignore those thoughts and feelings. I wanted it to be okay.
I just had to make it to Friday and we could hear the heartbeat.
I had been spotting dark brownish blood off-and-on since the incident at the vet. On Tuesday evening and Wednesday during the day, it became more of a light flow, period-like bleeding with small clots. On Wednesday evening, I felt cramping again in the lower abdomen, but this time, I noticed a pattern… an ebb-and-flow to its intensity. I rested. I told the kids I couldn’t do all the things they needed because I just needed to be in bed. After they went to sleep, I began to pass big clots. The first was the size of a mango, but flat. I was scared that it was the baby at first so I pulled it to the edge of the toilet with a spoon to examine it. It was just thick clotting with somewhat of a lining on it. It reminded me of a small liver. I continued to fill the toilet with blood and clots. I knew it wasn’t a good sign. The cramping continued. A few hours later, I had that feeling of needing to pass another clot. I could feel its decent through my canal. I quickly hopped up to get to the toilet. I made it just in time to pass several more large clots. While sitting there I passed… the baby.
It dangled from the umbilical cord, so I was able to pick it up with toilet paper to hold in the palm of my hand. It was still warm with its tiny hands up covering its eyes. The intended parents had told me just that day that it was a baby girl. My heart was sad for them… for her life cut so short. I didn’t know what to do with her. I couldn’t just flush it… my god!!! This is a life!!! I happened to have an empty toilet paper roll that could be used as a stable container. I slid her in there for the time being. I knew that I needed to pass the placenta but wanted to grab my phone to inform the surrogacy agent that I had for sure experienced a miscarriage. I waddled to get my phone while holding toilet paper between my legs as I was still actively bleeding. I sat back on the toilet and sent the heartbreaking message. It was 12:37am.
I was somewhat in shock that it was over. That’s it. This life was gone. I was disappointed that I couldn’t give that gift to those hopeful parents. I failed and their baby girl was no more. I sat there for awhile just stunned (and knowing I had to get more out of my body).
Trauma
I’m glad I had gotten my phone when I did because it may have just saved my life. Now I preface this by saying that calling for help was a huge step for me. I wouldn’t have done it unless I felt it to be absolutely necessary. I thought I would just wait for the rest to pass naturally, then I would be fine because that’s what (I read) usually happens with a miscarriage. Yet, perhaps it was because it was 15 weeks that made the difference or perhaps it was because it may have been unviable for weeks and my body had time to break- a lot- down the tissue, thus forming massive clots. I don’t know. But what I do know is that the way I felt was not normal.
I began to feel extremely light headed, nauseous, tingly, and as if I could pass out. I knew that if I tried calling for my oldest (sleeping) kid, he wouldn’t hear me over the fan with the door shut. But I knew I needed to talk to someone. At first I thought, “maybe the hospital has an emergency nurse line.” But when I found the number for the hospital, something inside told me not to call that number…. call 911. My internal struggle asked if it was truly an emergency. The answer was yes. The woman on the line confirmed my information and sent the paramedics. I waddled again with toilet paper to the door so I could unlock it and turn the porch light on. It only took about 3 minutes for them to arrive. I was waiting for them on the toilet again with only my shirt on since I had saturated my clothes already.
Silver-lining: It’s not everyday a single woman gets to have 6 or 7 good looking firefighters and paramedics in her house while she’s naked….. If only those men could have been there under different circumstances.
The lead EMT saw how much blood I had lost- along with the drop in blood pressure- and made the call to take me to the hospital. They asked if anyone was there and I told them my three kids were sleeping. I let them know that I would tell my 12 year old son that he would be in charge when they got up and to help get the girls off to school. The wheeled me to the ambulance on the gurney and off we went to the hospital. It was a bumpy ride so the EMT had difficulty putting a line in me. He decided to wait until we got to the ER. Once there, it was a few minutes wait due to being overcapacity with COVID and other cases. Thankfully, I was able to snag a mask from the ambulance before entering the ER. While we waited, I could feel my body systems losing control. The tingling and lightheadedness were becoming extreme with each passing moment. My blood pressure kept dropping to critical levels. The EMT must have noticed something because he eventually started trying to get the line of fluids in me right in the hallway. It wasn’t until I had the saline that I started to feel safe again.
Throughout the night, I kept passing clots and soaking my bedding. It must have been around 3 or 4 am when the OB on call came down and leisurely gave me the option of 1) pills to help the placenta pass or 2) D&C surgery to clean the uterus out. She left the decision completely up to me without any professional opinion or advice. Therefore, I chose the least invasive option: the pills. I took them and began to massage my abdomen to assist with the process. After the shift change in the early morning, another OB came to my area and began to scold me, “You are refusing a D&C!!! Why are you doing that?” I explained that I never refused it but that she only gave me the options and I chose the least invasive. If she would have said that it was necessary, then of course I would have done it! The OB was like, “Oh. Okay. Well then we are scheduling the surgery.” The first OB must have been nearing the shift change and wanted to avoid the paperwork… I get it. But please… if you are a doctor… please tell me what you think is necessary so I can make that decision with all the facts! We could have avoided more blood loss. I was told after the surgery that they tried three different heavy medications to stop the bleeding but that nothing was working! My body wasn’t responding to them; thus my bp continued to be low (not so much at the critical level but it stayed around 90s/50s) and my red blood cell count was dropping (10 g/dl at arrival, then 7.6 g/dl prior to the D&C). That may have been avoided with the OB’s professional opinion and not leave it up to the patient.
I continued to lay there switching from uncontrollable shivers with the fluid to lightheaded, tingly hot flashes when it would run out. I felt so dehydrated and couldn’t get enough water. I felt awful asking for help since they are understaffed during this time. I thought the people in the other beds needed help more than me. I knew that some nurses hadn’t had a break or lunch their entire shift. They dealt with physical restraints and COVID patients who wouldn’t listen to keep their masks on. I felt like I was wasting space…. taking up a much needed bed. When I saw the doctor again, I asked if I could have prevented this by coming to the emergency room before the miscarriage. They said “no, we would have told you to go home because you weren’t in an active miscarriage state.” I asked if I did the right thing by calling because I didn’t want to waste resources if it hadn’t been necessary. They reassured me that I definitely needed to call and be brought in because I could have easily died if I didn’t. This was not a situation that would have resolved naturally at home. After that, I felt like much less of a burden.
At 9:30 am they transferred me to the pre-op department. They explained what would happen during the surgery but that I wouldn’t remember it because I would be under anesthesia. At 10am, I was in the operating room. They didn’t put me under until they saw the doctor in the room (A little hospital insider for you: Apparently there are a few doctors who are notoriously late and the nurses have learned not to get patients or start procedures until they “see the whites of his eyes.” I got to be a part of their inside joke during my time in recovery as they waited for- not mine- but another surgeon).
I could feel cleared out but I also felt groggy and couldn’t see straight when I woke up. It must have been about noon or 1pm when I did. The surgery was only supposed to take roughly 30 minutes but I forgot to ask how long I actually took. Perhaps that is when they gave several different meds to stop the bleeding? I spent the entire day in recovery in the surgical unit. I was initially going to be discharged around 4 or 5 pm; however, when they took my blood, it came back at 5.1 g/dl, which is a critical level. There are concerns of cardiac arrest and death when it drops below 6-8 g/dl. I was extremely pale and still dizzy/tingly. They ordered 2 bags of blood for a transfusion.
The nurses and doctors that passed by would comment on my color returning and how I was looking so much better. The process takes about 4 hours so I wasn’t able to go home until the evening. They ordered me a delicious-because-I-hadn’t-eaten-in-24-hours meal of salad, BBQ chicken, brown rice, and corn (It actually tasted like old people but I didn’t care at that point). I also had a Sprite, jello, saltines, and applesauce before that arrived. I sure was hungry!
When my final blood test came back after the transfusion, the level was back up to 7.9 g/dl. Even though it showed that I was still anemic, it was a safe enough level for me to continue my recovery at home. The recovery nurse told me to take it easy on bedrest because it would be a while before I recovered from being severely anemic.
I was finally discharged around 8 pm to my brother’s care. Even though I asked the EMT to bring the fetus, he didn’t so I had my brother stop by my house so that the hospital could properly care for its disposal and run any needed tests in the pathology department. When he arrived, my recovery nurse and I hugged and expressed our joy in that we were able to spend the day together, despite the circumstances. He drove me home and helped me to my bed. The girls were spending the night at the neighbor’s but my son was home to greet me. My brother stayed the night to ensure that I was safe and even made me a high protein breakfast in bed. I am so grateful for the support of my two neighbors with helping the kids get to school and cared for when they got home. I am also grateful of the love of my family- especially my brother- who has been tirelessly doing all he can to help me recover.
God is good. I am blessed to have been gifted more days with my family and friends.
Another Chance at Life
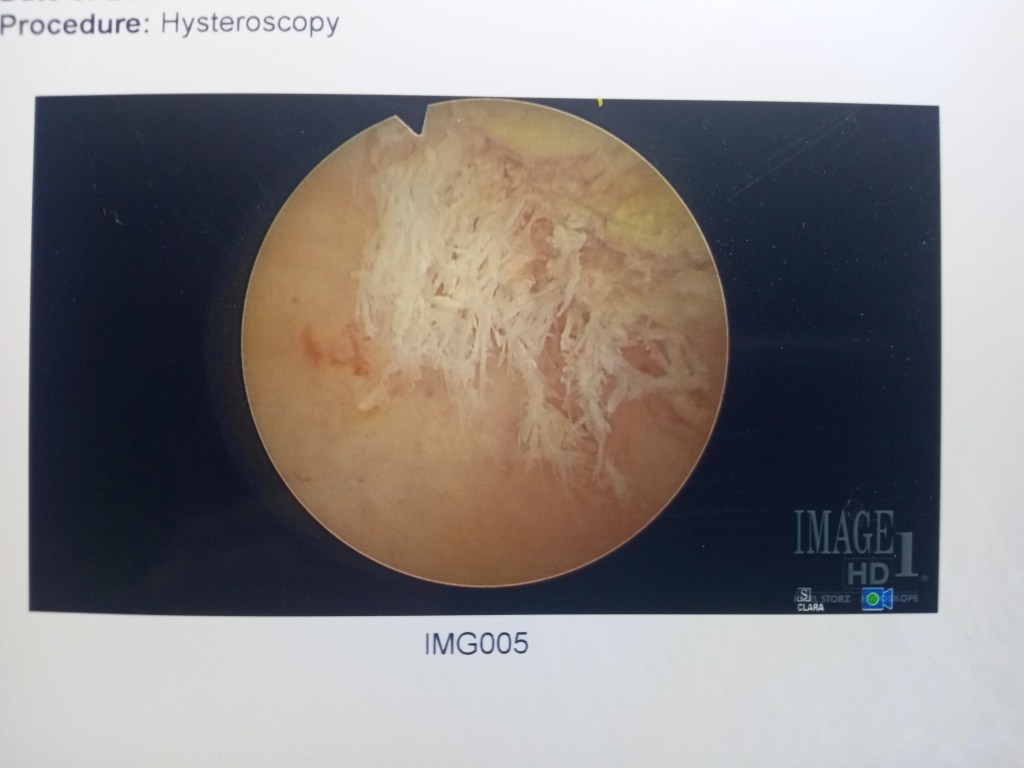
After careful consideration and talking with three doctors about the risks, I have decided to try again. At first, I wasn’t sure if I’d be able to because my uterine lining wasn’t perfect. The sonohysterogram (using soundwaves to get images from inside the uterus) showed some bumps on the hysteroscopy which were possible cysts. I was scheduled for surgery (hysteroscopy: light tube used to assist in precision surgery to remove debris from uterus). It turns out that some of the placenta from the miscarriage remained attached and needed to be scraped off. Now, I am back on the cycle of pills and needles.
I’ve already started to feel the absent-mindedness from the estrogen tablets, but thankfully I am prepared with pill boxes and highlighter to mark off when I’ve taken them.
Baseline ultrasound and bloodwork: Cleared
Follow-up ultrasound and bloodwork: Complete
Day-before bloodwork: And we’re off.
Frozen Embryo Transfer #2: 2/8/2022
Let’s Grow!
The second transfer was a success. The journey was similar to the first except the fatigue seemed worse. When I think about having any more kids, I have to say, my body could not take the fatigue of the first trimester. Other than that, it was smooth sailing. I really didn’t have much to share that wouldn’t have been redundant. Yes, I had minor complications but nothing life-threatening: I was diagnosed with iron-deficiency anemia. However, some studies claim that this is a natural occurrence during the second and third trimesters as the body prepares for birth. Iron levels decrease during pregnancy, but perhaps mine were a little too low. But man, the ferrous glutamate really did a number on me. If I took it during the day or without food, it caused nausea and upset stomach. If I took it at night instead, it caused dizziness and almost like a vertigo. I found that if I took it once every three days, it wouldn’t have the negative effects. I may have been experiencing iron toxicity by taking it daily. Ferrous sulfate was better because there weren’t such negative effects. The hematologist suggested injections, but I did not receive them in time for delivery (Spoiler Alert! I delivered this time!). Even though the doctor prescribed iron supplements, I tried Blackstrap molasses instead along with a vegan protein shake because I believe food is the best source for micronutrients. However, I did have extra protein in the urine at the time of delivery, which impacts the kidneys. I was downing pure cranberry juice to relieve that low back kidney pain and UTI when I got home. TMI right! Anyway, fast forward to the birth week.
The obstetrician scheduled me for induction at my Week 39 mark because I had already measured at 3cm and 70% effaced during my appointment the week before. He didn’t think I would make it to the next Thursday for the induction, but it was the soonest he could make it happen. Well, that sent my anxiety level through the roof! The one thing about the journey that I worried about was not making it to the hospital because my water broke, or I went into labor. Needless to say, I didn’t sleep much after that in fear that I would start labor in the middle of the night, have to deliver it myself at home (again), and the parents wouldn’t get to be a part of the delivery. Each day went by with no contractions. I made it to my Week 39 mark: The day of induction.
During the routine non-stress test that I had been having twice a week for the last few months with a $30 co-pay each time (thankfully I was reimbursed because THAT is just ridiculous!), there was one Braxton-Hick contraction that I didn’t even feel. Then, during the morning appointment at my doctor’s office, the midwife informed me that the hospital had been extremely busy and there were six women ahead of me, so she was able to confidently say I wouldn’t be going in that night.
Induction
The directions were to call each night for my status: The equivalent of jury duty for the L&D ward. Each night I was told to call in the morning when the next shift came on. Thursday night: No go. Friday morning and night: No room at the inn. Saturday morning: Nothing yet. Are they tired of hearing from me yet? Saturday night: “Sorry, nothing yet. But I may have beds soon when they transfer into recovery.” Two hours later (~10:30pm): “Good news. I have a bed! You have to be here by midnight to have it though. Do you want it?” I hesitated. What would the parents say? Thankfully they gave me a few minutes to call them before answering. I called the hospital back, “Yes! Let’s do this. I will be right over.” My mom drove me despite my resistance to accepting help. It was late. I wanted her to sleep and be there for the kids, but she wanted to be there for me instead. We checked into the hospital and completed any additional paperwork (not much, it was done before my arrival). I gave them the cord blood kit and they hooked me up to the IV. They explained that they would first give me the first round of a pill to help with dilation. Sometimes that would spark labor but if it didn’t work, they would give the second round then move on to the Pitocin. My only question: When do I need the parents up here!
I let the parents know that I wasn’t sure when it would happen but suggested they come up sooner than later. They were going to arrive around 6am since it takes a while to get it started but decided that they would arrive around 2:30am because they couldn’t sleep anyway. The intended mother came to the room, but the father took their son back to the rental. I had been tracking the contractions and confirming on the monitor. They were 10-15 minutes apart when the pill started kicking in. It didn’t take long before they were only 5 minutes apart and becoming more intense (~3:40am). However, I would breathe through them and wait for the next one. I don’t remember the specific time when I said, “Uh, my water may have just broke” but it was probably around 4am. I asked my mom to go ask a nurse to come check on me. When she arrived, she confirmed that it was my water and proceeded to check my dilation status. At that point, it was 8 cm. She pulled out and with her hand came a gush of fluids like someone forgot to turn off the faucet. She quickly went back in to check the baby and found its head floating upward a bit. This concerned her because the cord could easily wrap around the neck causing complications and potential injury to the long-term development of the infant. She yelled for help and requested that several nurses join her. Every time she would release her hand, Niagara Falls seemed to cascade over the rim of my bed and onto the floor. “In 14 years in L&D, I have never seen so much fluid when a water breaks!” commented one nurse. Once the flow had ceased, they wiped me up and changed my bed… ha! you thought I’d say bedding. Nope! They had to mop the floor and change the entire bed! Ah, never a dull moment with birthing a child.
After the excitement, the contractions really started to get intense. It became harder to breathe through them. Yet, I just had to focus on sending the energy to the uterus. Breath in deeply to fill the belly. As I breathe out, imagine that flow of energy going down my body into my uterus. Wiggle the toes for support. And…. the contraction is over. All I wanted was to be at 10 cm. Just tell me I’m at 10 because that means I can push.
When she said I was at 10cm, I was so excited, I had to double check: “So… I can push right!” I could already feel the decent of the baby getting closer to crowning and it was finally at those last points when the contractions become unbearable (without pushing) and you just want to take it all back. (Thankfully that period only lasted about 10 minutes).
It was the time. I could feel the urge to push, and I had gotten permission. (With my first, they said “Don’t push.” With my second, “Why aren’t you pushing?” With my third, I had to make the decision on my own since I had to do it myself. Now, I just wanted someone to tell me). Breathe through it. Push. Alternate. Breathe. Push. Hold your thighs and push. I felt the urge to poo which really makes you hesitant to push. Send energy to the uterus, not the bowels. Push…. without pushing out poo. Ah, I can feel the specificity of the baby again. I got past the feeling of defecation without embarrassment even though it is completely normal and natural. One last push… once the head comes out, a wave of relief that it’s “done” (even though it’s not).
The nurses had given the intended mother a gown. She watched the whole process and when the head came out, the midwife invited her to complete the delivery. With tears rolling down her cheeks, she gently eased her baby girl out the rest of the way at 4:50 am. After a few moments, they clamped the cord and handed her the scissors: “Would you like to cut the cord?” It was such a special moment for her. As they cleaned me up and figured out the complexity of the cord blood kit, the intended mother felt her baby skin-to-skin for the very first time.
And I… could finally rest. I was glad that it was over, and I could give this family such a precious gift. I was delighted that the mom was able to experience the completion of the delivery and feeling the skin-to-skin. But to be frank, I was glad to not be pregnant anymore. As promised, I had no inclination to have a baby of my own nor felt an attachment that would make me feel loss after it goes back with them. We had agreed that I would breast feed the infant for the sake of her immunity but also the benefits for my body. I did so within the first two hours and the mother was okay with me holding her to do it. When they had a room available, they transferred her and the baby to get some rest. They transferred me to my own room too. The next day, the mom, dad, brother, and baby came to visit my room and I was able to hold the baby for a little bit while we visited and reminisced about the experience. We also made plans to get together so that my kids could meet the baby too.
Of course, my middle girl was a mother hen and loved holding the baby (sorry for the blacked-out face on baby- I can’t post pictures of her via the contract). They jokingly told her she could be their live-in nanny back in their home country. I’m not sure that my youngest really knew what to feel. It may have been quire surreal for her, so she disappeared into her room. My son was a typical teenage boy who said hello then disappeared in his cave.
We finalized the process so they could get the birth certificate and passport. Then they were off to introduce their new addition to their family back home. We will keep in touch and share pictures of our families. But as far as the surrogacy journey:
Here is where the story ends.
It was an unforgettable adventure!
But I’m so thrilled to have my body and freedom back. One of the first things I did when I got home was enjoy a small glass of cabernet sauvignon. Thanks to my good friend who gifted it to me. Next on the list: Yoga and hiking!


I can’t believe what you went through. I too went through a similar situation when a surrogate. Is there an update to your journey?
LikeLike